Magnetic Anastomosis for Weight Loss
To understand how magnetic anastomosis works and why it’s so revolutionary, we need to know how combination restrictive and malabsorptive procedures, such as SADI, Duodenal Switch, and gastric bypass, function. In each case, the stomach is reduced in size by surgical means. This is the restrictive portion of the procedure, which helps patients get full on a smaller volume of food. However, restriction alone is insufficient when patients need to lose a significant amount of weight, as evidenced by the limited weight loss achieved with the now-rarely used Lap-Band. In some bariatric procedures, including the gastric sleeve, SADI, and duodenal switch, the removal of the upper outer portion of the stomach, known as the fundus, provides hormonal benefits by eliminating most ghrelin production (a hormone associated with hunger). That said, procedures that bypass part of the small intestine, creating malabsorption, have a knack for resetting gut bacteria and releasing gut hormones, which can be precisely what the patient needs to improve insulin resistance and get back on track even before they lose a significant amount of weight.
Until now, during the bypass portion of the procedures mentioned above, surgeons have used intricate suturing techniques to reattach the parts of the small intestine. While this suturing process is very safe and effective in the hands of a skilled surgeon, there is always added risk. However, new technology may be changing that.
Enter Magnetic Anastomosis
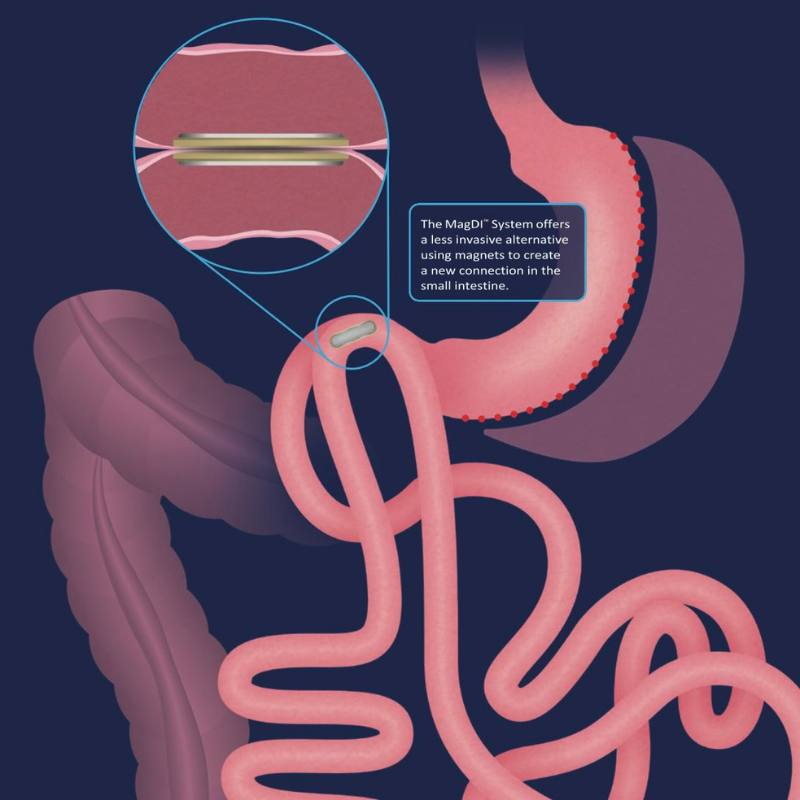
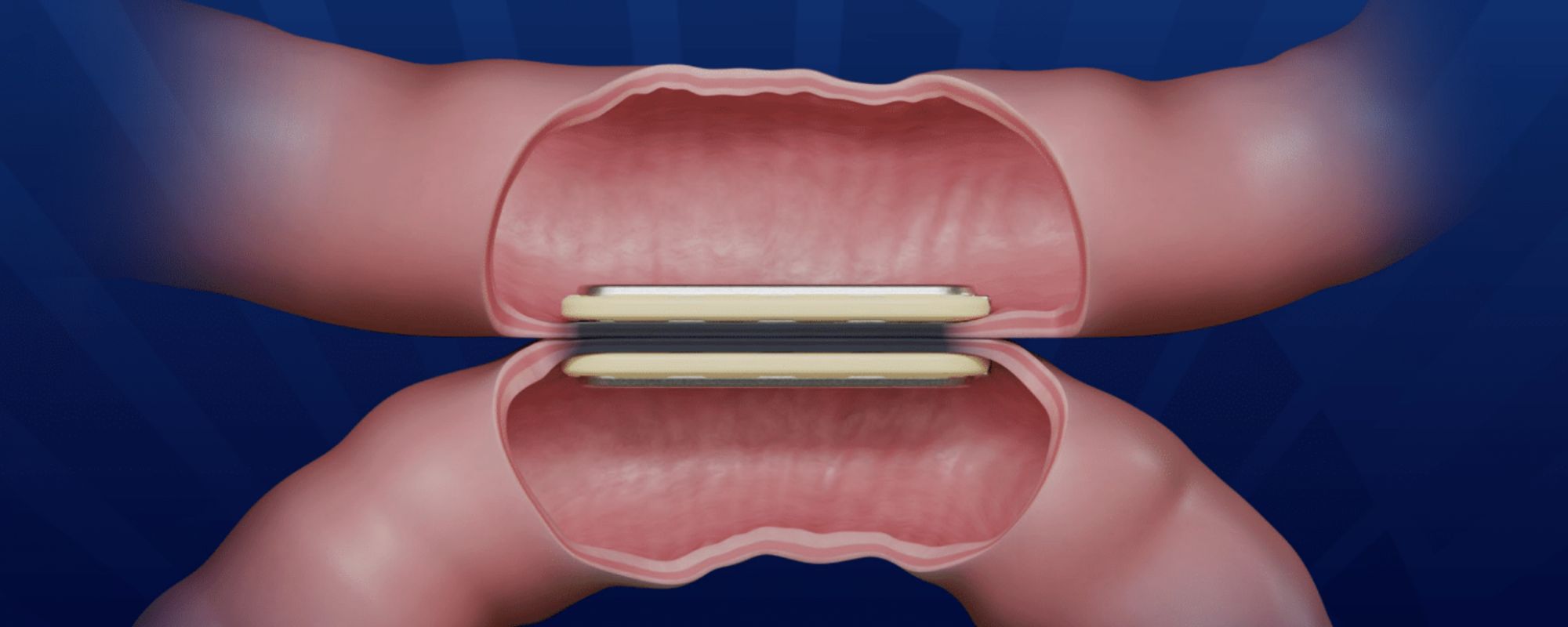
Magnetic anastomosis involves the minimally invasive placement of two small but strong magnets in the small intestine.
The procedure begins with the patient swallowing a magnet in the hospital’s outpatient department. After about two hours, the magnet will have traveled through the stomach and duodenum and will have settled in the 2nd or 3rd portion of small intestine. With the assistance of a minor laparoscopic procedure, we direct this first (swallowed) magnet to meet its pair that is introduced endoscopically (non-surgical, through the mouth). At this point, we position the magnets precisely where needed, about 2cm below the pylorus or outlet valve from the stomach.
When ready, the intestines are joined using the magnetic force. After 4-6 weeks, the magnetic compression erodes through the intestine, and the body naturally fuses the tissue, creating a tight seal with no leaks or need for sutures.
Once the magnets have eroded through the intestine, they stay together, drop into the G.I. tract, and are expelled through a natural bowel movement. If the magnets need to be retrieved, we can do so once again using endoscopic, non-surgical means.

Our Experience with Magnetic Anastomosis
Our practice has been at the forefront of using magnetic anastomosis technology in advanced bariatric and metabolic surgeries. We’ve incorporated this innovative approach in our SADI procedures, helping improve surgical efficiency and patient outcomes.
Our team performed our first cases in Montreal in September of 2024 and introduced the procedure on the East Coast in December 2024. Since then, we have ranked among the highest-volume practices in the country that utilize magnetic anastomosis.
Further, Dr. Enochs serves as one of the few U.S. proctors for the magnetic device, having trained surgeons across the United States and the Middle East, and has presented on this topic at major national and international conferences, including the American Society of Metabolic and Bariatric Surgery, the International Bariatric Club, and the International Federation for the Surgery of Obesity and Metabolic Disorders.